Cataract
Cataract is the slowly progressive opacification of the natural clear lens of the eye. The lens has a major role to play in focusing the light rays on to the retina and helping us see clearly. As the opacities progress, they interfere with the quality and quantity of vision.
Causes of Cataract Formation
Most of the cataracts are the result of aging, but there could be other causes like:
- Trauma to the eye and electric or heat injuries can result in cataracts.
- Previous posterior segment eye surgery
- Medicines like steroids, when used for prolonged periods, can also lead to cataract formation.
- Prolonged inflammation in the eye
- Radiations like X-rays, UV-B rays, microwaves can all cause cataracts
- Cigarette smoking is strongly associated with cataracts
- ongenital cataracts (babies born with cataracts) may result from intrauterine infections or inborn errors of metabolism.
- Genetic disorders like Down’s syndrome, Edward syndrome etc.
Risk factors for development of early cataracts include diabetes, smoking tobacco, prolonged exposure to sunlight, and alcohol (controversial).
Symptoms
The exact symptoms depend on the type of cataract. The common ones are, diminished vision with frequent change in glasses, glare and haloes at night and yellowing of vision. With nuclear cataracts, the near vision seems to improve accompanied by a drop in distance vision.
Diagnosis
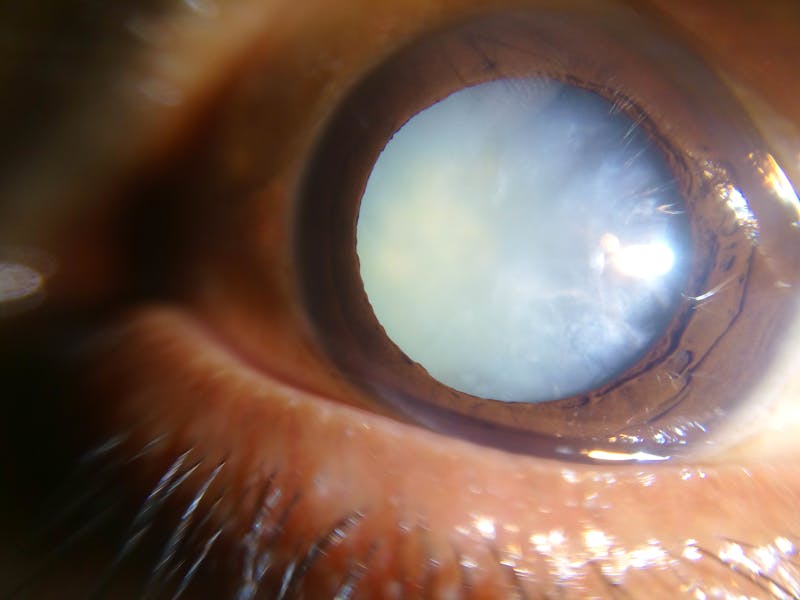
A simple eye examination on a slit lamp is enough to diagnose visually significant cataracts. Mature cataracts (white cataracts) are easily visible on diffuse light examination also.
Treatment
Surgery is the only treatment for cataracts. Following types of surgeries are available:
- Phacoemulsification is the most widely used cataract surgery in the developed world. Through two small incisions made in the periphery of the clear cornea, the cloudy lens is emulsified using ultrasonic energy and then aspirated, leaving the capsular bag in place. A permanent, foldable Intra ocular lens is then placed inside the capsular bag. Since the corneal incisions are small they are self-sealing, therefore no sutures are required. There are very few post-operative precautions and patient is ambulatory on the day of the surgery. Some eye drops need to be used for a few days after the surgery.
- Extracapsular cataract extraction (ECCE) consists of removing the lens manually, but leaving the majority of the capsule intact. The lens is expressed through a 10- to 12-mm incision which is closed with sutures at the end of surgery. It has a longer post-operative recovery period, with patching of the eye for few days. The vision takes longer to stabilize compared with phacoemulsification. ECCE is less frequently performed than phacoemulsification, but may be used when dealing with very hard cataracts or other situations where phacoemulsification is not possible.
- Manual small incision cataract surgery (MSICS) has evolved from ECCE. In MSICS, the lens is removed through a self-sealing scleral tunnel wound which, ideally, is watertight and does not require suturing. The incision is markedly larger than that used in phacoemulsification. This surgery is popular in the developing world where access to phacoemulsification is still limited.
The natural cataractous lens is replaced with an artificial lens, known as an intraocular lens (IOL), which remains permanently in the eye. Intraocular lenses are usually monofocal, which is correcting for either distance or near vision. Glasses are needed after monofocal IOL implants. With the advent of multifocal lenses the patient has the option to improve near and distance vision simultaneously. The type of lens to be implanted depends on a number of factors and is decided on a case to case basis after discussion between the surgeon and the patient.
Risks and benefits
The present day surgical techniques and surgical skills result in excellent visual results with shorter recovery times and comfortable post-operative period.
As with any surgery, there are some risks involved. Many of these complications can lead to a delay in recovery of the eye. Some of them may require further operations or treatment and therefore further follow up appointments.
During surgery
Most of the cataract surgeries are performed under peribulbar anesthetic block (injection of the anesthetic next to the eye ball). Rarely this may result in retrobulbar hemorrhage (bruising behind the eye). The surgery then has to be postponed. The rapidly expanding blood may lead to loss of vision due to pressure on the eye nerve. In extremely rare cases, during the local anesthetic injection, it is possible for the eye to be punctured by the needle. This can lead to retinal detachment, bleeding or loss of vision.
Accidental formation of hole in the posterior capsule (on which IOL is placed), will lead to additional steps and prolonged surgery with delayed visual recovery. It may predispose to retinal detachment, macular edema (fluid in central retina) and chances of cataract pieces falling into the back of the eye. Sometimes when there is a posterior capsular tear, the IOL has to be placed at a different site during the same surgery or at a later date.
Bleeding during the surgery can lead to sudden loss of vision.
Following Surgery
Corneal edema (collection of fluid in corneal layers with clouding and decrease in vision) can develop after surgery. This may resolve with prolonged use of eye drops or require corneal grafting at a later date.
Endophthalmitis, is a serious infection inside the eye. The treatment involves further operation(s) to take samples and to allow injection of antibiotics into the eye. Treatment has to be very prompt for it to be effective. Very rarely does an eye need to be removed because of this infection.
Excessive inflammation may develop after surgery. Though uncommon, it will require an increase in strength or frequency of steroid drops; or steroids may need to be given by injection or orally.
The intraocular pressure (IOP) may rise, requiring the use of pressure lowering eye drops or pills.
Cystoid Macular edema – This is swelling in the center of retina and can occur in 1- 5% of patients within the first few weeks of cataract surgery. This leads to blurred vision. The treatment is with additional anti- inflammatory eye drops for a few weeks, or sometimes a steroid injection next to the eye. In most patients, it settles down with no lasting effect.
Despite an uncomplicated eye surgery, some patients may notice glare, halos, reflections or a feeling of blurred vision or discomfort. Eye examination is generally normal and these symptoms usually become less obvious with time. They can neither be prevented nor can they be treated.
Cataract surgery may worsen pre-existing eye conditions, such as glaucoma, uveitis (inflammatory eye disease) or corneal diseases.
Rarely, the lens implant may dislocate into a wrong position, with time. This may require surgical correction.
DISCLAIMER
This web page provides general information and discussions about health, medicine and related subjects. The information and other content provided on this website, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.
The content is for information purpose only and is not a medical advice. Qualified doctors have gathered information from reputable sources; however Credence Medicure Corporation is not responsible for errors or omissions in reporting or explanations. No individual should use the information, resources and tools contained herein to self diagnose or self treat any medical condition.
If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately.
The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution. Credence Medicure Corporation gives no assurance or warranty regarding the accuracy, timeliness or applicability of the content.
