Glaucoma
Glaucoma is a group of conditions that results in optic nerve damage, manifesting as visual field loss. Peripheral vision decreases first, followed by central vision, ultimately resulting in permanent blindness, if not treated. It is the leading cause of irreversible blindness, globally. It has been estimated that 60.5 million people were affected by primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG) globally in 2010.
Types of Glaucomas
Broadly speaking, glaucomas can be classified as primary or secondary. Then there are childhood glaucomas. Primary means when there is no clear precipitating factor and secondary means when an underlying cause, like injury, previous surgery, cataract etc. can be identified.
Primary Glaucoma:
- Primary Open Angle Glaucoma (POAG): This is the most common type of glaucoma. This is caused by the slow clogging of the drainage canals, resulting in increased eye pressure. The eye ball has a wide and open angle between the iris and cornea. Patients are mostly asymptomatic. Most of them are discovered on routine eye examination. At one end of the disease spectrum are patients with glaucomatous damage associated with high IOP and at the other end of the spectrum are those with glaucomatous damage associated with IOP in the normal range (Low Pressure or Normal Tension Glaucoma).
- Primary Angle Closure Glaucoma (PACG): This is caused by blocked drainage canals, resulting in a rise in intraocular pressure. The eye ball has a closed or narrow angle between the iris and cornea. Acute angle closure glaucoma presents with a painful red eye with sudden drop in vision and haloes around light. The patient has a very high IOP which needs to be lowered emergently, to prevent permanent loss of vision.
Secondary Glaucoma:
- Exfoliative Glaucoma occurs when a flaky, dandruff-like material peels off the outer layer of the lens and clogs up the drainage system of the eye and causes the IOP to rise. This produces pseudoexfoliative glaucoma.
- Neovascular Glaucoma is caused by the growth of new blood vessels on iris and over the drainage channels of the eye causing a rise in IOP. This type of glaucoma is always associated with other abnormalities, most often diabetes.
- Pigmentary Glaucoma occurs when the pigment granules from the iris (the colored part of the eye) break into the clear fluid (Aqueous Humor) produced inside the eye. These granules slowly block the drainage channels, causing the IOP to rise.
- Traumatic Glaucoma — Injury to the eye may result in angle closure or open angle type of glaucoma and can occur years after the injury.
- Uveitic Glaucoma — Uveitis is swelling and inflammation of the uvea, the middle layer of the eye. Glaucoma can result because of the inflammation itself or the steroids used to treat it.
Childhood Glaucoma:
These is a group of glaucomas that may present anytime from birth till the teenage years. Those presenting at birth are said to have Congenital Glaucoma. Infantile Glaucoma is diagnosed when the presentation is made anytime between birth until 3 years of age. When the diagnosis is made between 3 years of age to teenage years, it is called Juvenile Glaucoma.
Risk Factors for Glaucoma
- High Intraocular Pressure (IOP): Raised IOP is the most important risk factor for developing glaucoma. Ocular hypertension, an intraocular pressure above the traditional threshold of 21 mm Hg, is not necessarily a pathological condition but it increases the risk of developing glaucoma. The higher the IOP, the more the chances of glaucomatous damage.
- Ethnicity: Angle Closure Glaucoma is more common among people of East Asian descent. This is because they have shallower anterior chamber depths. There is a higher prevalence of glaucoma in Inuit populations, compared to White populations, in Canada and Greenland. Adjusting for age, African-Americans are 3 to 4 times more likely to have glaucoma compared to Caucasians
- Genetics: Positive family history is a risk factor for glaucoma. The relative risk of having primary open-angle glaucoma (POAG) increases about two- to four-fold for people who have a sibling with glaucoma. Normal-tension glaucoma, which comprises one-third of POAG, is also associated with genetic mutations.
- Age: Increasing age is a risk factor, especially age over 60.
- Pre-existing medical conditions: Diseases such as diabetes, heart disease, high blood pressure and sickle cell anemia increase the risk of developing glaucoma.
- Refractive errors: Myopia (short sightedness) is an independent risk factor for open angle glaucoma. People with myopia have a 2–3-fold increase in the risk of developing glaucoma compared to non-myopic patients. Higher the degree of myopia, more the risk of developing glaucoma. People with hyperopia (farsightedness) tend to be more at risk for developing angle-closure glaucoma.
Symptoms
Most of the glaucoma patients are asymptomatic. Thus, the lack of clear symptoms make screening, via regular eye check-ups, important.
About 10% of people with closed angles present with acute angle closure. This is characterized by sudden onset of pain and redness in the eye, halos around lights and very high intraocular pressure (>30 mmHg), nausea and vomiting associated with sudden decrease in vision, and a fixed, mid-dilated pupil. Patients with chronic angle closure glaucoma may have a history of episodes of blurring of vision with haloes around light, with spontaneous resolution (intermittent angle closure).
Diagnosis
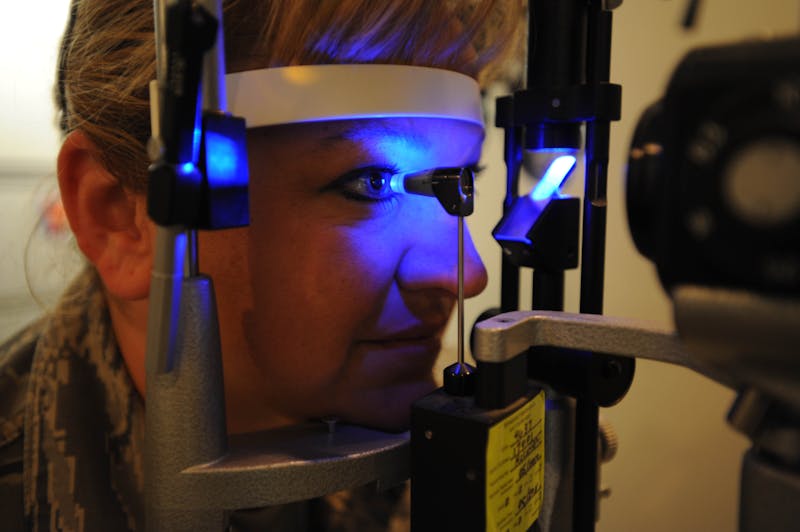
Since patients are largely asymptomatic, screening for glaucoma is usually performed as part of a standard eye examination. Both optometrists and ophthalmologists can screen for glaucoma. The tests include measurements of the intraocular pressure by tonometry; gonioscopy to assess the anterior chamber angle and a detailed examination of the optic nerve head to look for any visible damage to it.
Visual field testing is required in all those suspected to have glaucoma. Early glaucoma damage can be assessed by analysis of retinal nerve fiber layer thickness. This can be done by imaging techniques such as optical coherence tomography, scanning laser polarimetry, and/or scanning laser ophthalmoscopy. Though visual field loss is the most specific sign of glaucoma, it follows a decrease in the retinal nerve fiber thickness, and therefore occurs later in the course of the disease.
In those suspected to have glaucoma, a regular follow up, with testing, is mandatory.
Treatment
Early diagnosis and treatment is the key to preventing blindness from glaucoma. There is no permanent cure for glaucoma. Even surgery is not guaranteed to be effective lifelong. Although intraocular pressure (IOP) is only one of the major risk factors for glaucoma, lowering it by various pharmacological and/or surgical techniques is currently the mainstay of glaucoma treatment. Following modalities of treatment are used:
Pharmacological treatment: Most patients of glaucoma are treated with eye pressure lowering eye drops that need to be used lifelong. Tablets are also available for short term use, to immediately lower the IOP. Intravenous osmotic agents sometimes need to be used for immediate lowering of very high IOP, as for example, in acute angle closure glaucoma.
Lasers: Argon laser trabeculoplasty (ALT) may be used to treat open-angle glaucoma, but this is a temporary solution, not a cure. Selective Laser Trabeculoplasty (SLT) is another type of Laser used for temporary lowering of IOP in open angle glaucoma. Whereas surgeons typically perform ALT after medical therapy has failed and prior to surgical intervention, SLT may be appropriate as primary therapy for some patients with open-angle glaucoma.
Nd: YAG laser peripheral iridotomy (LPI) is used in patients susceptible to or affected by angle closure glaucoma or pigment dispersion syndrome. A full-thickness opening is made with the Laser in the iris, to equalize the pressure between the front and back of the iris, thus correcting any abnormal bulging of the iris. In some cases of intermittent or short-term angle closure, LPI may lower the eye pressure. An LPI also reduces the risk of developing an attack of acute angle closure. In most cases, it also reduces the risk of developing chronic angle closure.
A transient rise in IOP is expected after Laser.
Surgery: There are different types of glaucoma filtration surgeries. All the surgeries essentially increase the aqueous outflow from the eye ball. This results in a decrease in the IOP. Surgery is the first line of treatment in most of the childhood glaucomas. In adults, surgery is generally done when other modes of treatment have failed.
The most common conventional surgery performed for glaucoma is trabeculectomy. Traditionally, chemotherapeutic adjuvants, such as mitomycin C (MMC) or 5-fluorouracil (5-FU), are used with trabeculectomy to prevent scarring of the surgical site, which can lead to failure of the surgery.
Another type of surgery is the Glaucoma drainage implants. These are indicated for glaucoma patients not responding to maximal medical therapy, with previous failed conventional surgery (trabeculectomy).
Although the surgical approach to childhood glaucoma varies around the world, surgery on the angle remains the preferred initial approach for primary congenital glaucoma and a major advance has been the concept of incising the whole of the angle (circumferential trabeculotomy).
Cyclodestructive procedures: In cyclodestructive procedures, the secretary epithelium of the ciliary body is damaged, which leads to reduced aqueous humor secretion and lowering of IOP. Because the ciliary epithelium can regenerate, multiple treatments are necessary in some patients to achieve the desired long term IOP lowering effect.
The different modalities to achieve cyclodestruction are diathermy, surgical excision, cryotherapy, ultrasound, and laser light. Diode laser cyclophotocoagulation is preferred over the other modalities.
Chronic hypotony (IOP<6mmHg) and ultimately phthisis bulbi (atrophy, shrinkage, and disorganization of the globe) can be a complication of excessive cyclodestruction.
Complications of Glaucoma Surgery
Though glaucoma filtration surgery has an improved safety profile, because of improvement in techniques, it can still be fraught with complications, which include the following:
-
Intraoperative and postoperative suprachoroidal hemorrhage: This is bleeding in the layers of the eye ball that are present at the back. This hemorrhage is a serious complication that can be seen during or after any intraocular surgery. If it occurs during the surgery and cannot be controlled (i.e., expulsive hemorrhage), it can lead to loss of vision. Postoperative suprachoroidal hemorrhage usually occurs within the first week after glaucoma surgery and is generally associated with postoperative hypotony (IOP<6mmHg).
-
Intraoperative complications of filtration procedures: Conjunctival buttonholes and tears can lead to failure of bleb formation and a flat anterior chamber. Vitreous loss during glaucoma surgery is not very common but it can predispose to complications like corneal edema, epithelial down growth, uveitis, retinal detachment, cystoid macular edema, and endophthalmitis (infection of tissues or fluids inside the eye). The vitreous can mechanically plug the sclerostomy (surgical site), leading to filtration failure.
-
Hyphema: Hyphema is blood in the anterior chamber of the eye. It generally occurs during surgery or within the first 2-3 days after surgery. In most cases, no treatment is necessary, and the blood is absorbed within a brief period of time. Surgical drainage of blood may be considered on a case to case basis.
-
Hypotony: Possible complications of hypotony include, flat anterior chamber, gradual failure of the bleb (failure of surgery), visual loss, cataract, corneal edema, Descemet membrane folds, choroidal hemorrhage, hypotony maculopathy, chorioretinal folds
-
A flat anterior chamber with an elevated or normal intraocular pressure (IOP): This could be related to suprachoroidal hemorrhage, aqueous misdirection, and pupillary block
-
Visual loss: Unexplained loss of the central visual field “wipeout” after glaucoma surgery is rare. Older patients with advanced visual field defects affecting the central field with split fixation are at an increased risk.
-
Bleb related complications: e.g., bleb leaks, early and late failure of filtering blebs, encapsulated blebs, symptomatic blebs, and bleb-related eye infection (which could be early or years later).
-
Endophthalmitis: This is infection of the inner tissues and fluids of the eye. It is one of the most serious complications following intraocular surgery. In the setting of glaucoma surgery, the risk of endophthalmitis extends well beyond the immediate postoperative period. Endophthalmitis requires immediate attention,
Summary
Glaucoma is a silent thief of vision. A heightened awareness amongst the ophthalmologists and optometrists is necessary, so that screening for glaucoma is part of the routine eye checkup. Awareness also needs to be created among the general population, so that they go for a routine eye checkup periodically, especially after the age of forty. The American Academy of Ophthalmology (AAO) recommends that patients without risk factors for eye disease should have comprehensive eye exams at the following intervals:
- Under 40 Every 5 – 10 years
- 40 – 54 Every 2 – 4 years
- 55 – 64 Every 1 – 3 years
- 65 or older Every 1 – 2 years
The AAO also suggests that people who are at risk for glaucoma have complete eye exams according to the schedule below:
- Ages 40 to 54, every 1 to 3 years
- Ages 55 to 64, every 1 to 2 years
- Ages 65 and older, every 6 to 12 months
DISCLAIMER
This web page provides general information and discussions about health, medicine and related subjects. The information and other content provided on this website, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.
The content is for information purpose only and is not a medical advice. Qualified doctors have gathered information from reputable sources; however Credence Medicure Corporation is not responsible for errors or omissions in reporting or explanations. No individual should use the information, resources and tools contained herein to self diagnose or self treat any medical condition.
If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately.
The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution. Credence Medicure Corporation gives no assurance or warranty regarding the accuracy, timeliness or applicability of the content.
